About 9-14% of people in Africa have some form of osteoarthritis (OA).1 For most people, the earliest
signs of osteoarthritis come as a whisper- usually, a stiff knee when they wake up, achy hip after long
walks, or fingers that don’t entirely move as they used to. Osteoarthritis is usually seen in people over
45, but it can also affect the young. When the symptoms begin, it’s very easy to trivialize these changes
and chuck them down to ageing. However, as time passes, the whispers become a bit louder and louder,
resulting in discomfort, swelling around the affected joints and an insidious loss of function that can
significantly impact your daily life.
We see patients with arthritis every day, and we know first-hand how frustrating and overwhelming it
can be to navigate this condition. Whether you have only recently being diagnosed or you have been
living with OA for many years, it is important that you understand what’s going on in your joints, how
you can manage your symptoms and what treatment options are available to you.
So, what is Osteoarthritis?
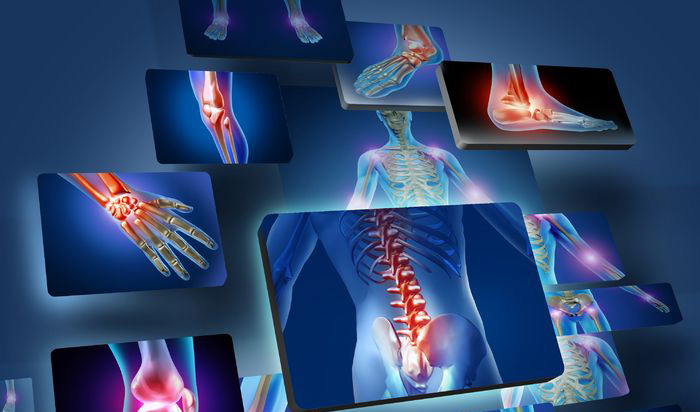
Osteoarthritis is the most common form of arthritis, affecting millions worldwide. As was said in the
beginning, it is commonly referred to as “wear and tear” because it occurs when cartilage protection
that cushions the end of your bones that form your joints wears down over time. Our joints allow us to
do complex movements like bend, grasp, etc, and the cartilage is a cushion that absorbs shock and
prevents the bones from rubbing on each other. When you have OA, the cartilage breaks down and
sometimes floats inside the joint fluid. When the cartilage’s surface becomes rough, it causes pain and
stiffness. The body tries to heal itself by forming more bones. These bone spurs (called osteophytes)
are not always symptomatic but they can cause more pain and restrict the movement of the joint.
What causes or predisposes to OA?
For many people, it’s the ageing process, but for others, it is after trauma to the joint, genetics, being
overweight or obese, infection in the joint, overuse of the joint, or some other medical conditions. This
can lead to joint stiffness, pain, swelling, and, in more advanced cases, a change in the shape of the
joint. OA most commonly affects the knees, hips, hands, and spine but can also affect any other joint.
What Symptoms Should You Look Out For?
Different people may have other symptoms, but the most common that you may find are:
- Joint pain, especially after physical activity or at the end of the day
- Joint stiffness that is worse in the morning or sometimes after rest
- Swelling around the affected joint
- A clicking or grating sound when you move your knee
- Limitations in the range of motion of the joint that makes every day activities like walking or climbing stairs more difficult.
Diagnosing OA
To diagnose OA, we’d ask you about your medical history, examine the affected joint and limbs, and
finally request some imaging (e.g., x-rays) and blood tests, if necessary, to help us confirm the diagnosis.
What can you do?
Osteoarthritis is a chronic condition with many ways to manage it effectively. Usually, lifestyle changes,
medications, injections in the joint and sometimes surgery can help control symptoms and keep you
moving. Here are a few suggestions:
- Don’t stop moving: Although exercise isn’t fun when you have joint pain, movement helps to maintain joint function. Low-impact activities like walking, swimming, and cycling can help strengthen the muscles around the joint and provide better support while also reducing the pain.
- Losing or maintaining a healthy weight: Even a tiny amount of weight loss can lessen the pain significantly and slow down the progression of the disease, as excess weight puts pressure on your hips and knees especially.
- Manage the pain and swelling: Over-the-counter pain medications like paracetamol or nonsteroidal anti-inflammatory drugs(NSAIDs) like ibuprofen and diclofenac can help manage pain. Still, they should be used with caution and under medical supervision. Other options include topical creams, physical therapy, and even joint injections like Platelet-Rich Plasma (PRP) in some cases.
- Consider using assistive devices: Canes, braces and shoe inserts can help take some of the pressure off the joints and improve your capacity to perform everyday functions
- Surgical option: Suppose your pain worsens, affecting your quality of life despite conservative measures. It may be time to discuss surgical options such as joint replacement in that case.
Living Well with Osteoarthritis
A diagnosis of OA doesn’t mean you have to stop doing the things you love. You can continue to live
an active and fulfilling life with the right approach. The key is to listen to your body, make adjustments
as needed, and work with your healthcare team to find the best management plan for you.
Please get in touch with us if you’re struggling with joint pain and unsure what to do next. You deserve
to move freely and without pain. And remember, every step, no matter how small, toward better joint
health is worth taking.
References
Al Saleh J, Almoallim H, Elzorkany B, Al Belooshi A, Batouk O, Fathy M, Vainstein N, Kaki AM.
Assessing the Burden of Osteoarthritis in Africa and the Middle East: A Rapid Evidence Assessment.
Open Access Rheumatol. 2023 Mar 15;15:23-32. doi: 10.2147/OARRR.S390778. PMID: 36945659;
PMCID: PMC10024869.